You’re pregnant – hurrah – but suddenly there’s so much to learn. These include all the screenings and tests that you, as a pregnant woman, have to undergo. But don’t worry, we’re here to help.
Haemoglobin

Haemoglobin is a test to detect iron anaemia and indicates the need for vitamin and mineral supplementation during pregnancy. Blood is taken in early pregnancy and then repeated at 32 weeks. This test is recommended for all pregnant women.
Sickle Cell and Thalassaemia Trait
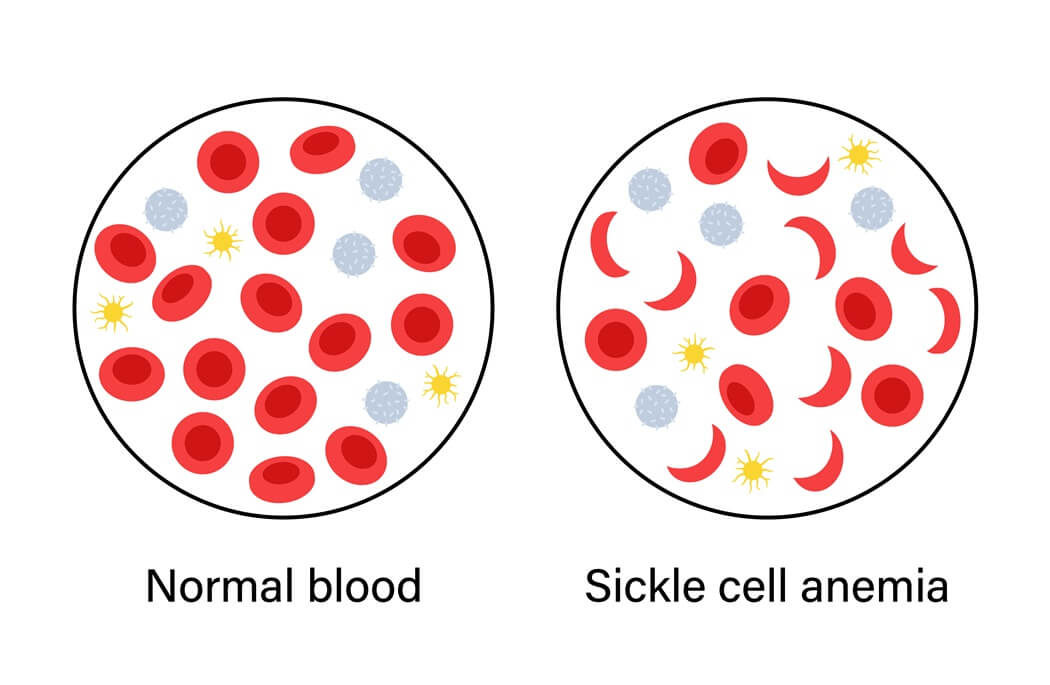
Sickle Cell and Thalassaemia are inherited disorders of haemoglobin evident in the mother’s and father’s blood. In pregnancies where both parents are carriers, the newborn baby may be anaemic.
Rubella (German Measles)
Rubella is a viral infection, which can exert harmful effects on the developing foetus in the first half of pregnancy. Screening is undertaken to assess the mother’s immunity to the virus. If there is no immunity to the virus, then a Rubella vaccination will be offered during the postnatal period.
VDRL (Syphilis)
Syphilis is a sexually transmitted disease which is now extremely uncommon.
Tay Sachs Screening

Tay Sachs is an inherited condition of fat metabolism. It is a recessive gene and if both parents are carriers, then the baby may be affected. A test can be performed on either parent’s blood before or during pregnancy. If the mother and father are carriers then an amniocentesis is advised to check the baby.
Blood Group and Rhesus – Antibody Screening

Blood is grouped and the presence of antibodies is assessed. The majority of antibodies are harmless, but a minority, particularly the Rhesus type may affect the foetus. If the mother is Rhesus Negative, the antibody screening will be repeated later in pregnancy. Women, who are Rhesus Negative will be offered an Anti-Dimmunoglobulin injection at 28 and 34 weeks in order to prevent Rhesus immunization. The injection may be repeated after birth, if the baby’s blood, taken from the placenta is Rhesus Positive.
Hepatitis

The Hepatitis virus may affect the mother’s liver and cause jaundice. Women who are carriers of this virus may transmit the infection to the baby. Screening for Hepatitis is routine.
Toxoplasmosis

Toxoplasmosis is an infection probably acquired from eating uncooked meat or from exposure to infected cat faeces. Infection during pregnancy is rare, but the effect on the baby can be serious. Toxoplasma antibodies will indicate when the infection was acquired. Infection before the pregnancy does not affect the baby.
Test in Pregnancy

It is recommended that all mothers consider an HIV (Human Immunodeficiency Virus) antibody test as part of their routine antenatal care. There are advantages to mother and baby of knowing HIV status. HIV is spread through unprotected sexual intercourse or needle injury. The HIV antibodies appear during the first three months following infection. HIV may ultimately lead to the disease called AIDS (Acquired Immune Deficiency Syndrome), but it is not a test for AIDS because the virus may remain dormant.
Discuss the test with your spouse and your doctor during your antenatal visits. The results will be kept confidential. There are advantages to having this test. Women at risk will know whether they are infected, and precautions can be taken to reduce the rate of transmission of the HIV virus to the baby. However, if the test is negative, the mother will be reassured.
Routine screening

Blood pressure monitoring and urine testing will be performed at each of your antenatal appointments. The main things that your doctor will be testing for is protein and glucose. The presence of protein in your urine can be associated with a urine infection. However, raised blood pressure and protein in your urine is of more concern if it is associated with visual disturbance, headaches, vomiting and sudden swelling of the ankles, face and hands. This could indicate pregnancy-induced high blood pressure known as pre eclampsia.
Pre-eclampsia is likely to develop in pregnancy if you have predisposing factors such as being over 40 years old, a family history of pre-eclampsia, if you have had pre-eclampsia in a previous pregnancy, a multiple pregnancy or a starting body mass index greater than 35.
The presence of glucose in the urine could indicate that a mother may be developing gestational diabetes. Confirmation blood tests can confirm pre-eclampsia and gestational diabetes.
Ultrasound scans

Before choosing whether to have a scan of your baby or not, understand that although scans in pregnancy are now common place, there is very little research relating to the positive and negative effects of scans. Many women and couples find seeing their baby on scan and/ or taking a photograph very reassuring. Depending on where you choose to have your antenatal ultrasound scanning the following options will be available:
Viability Scan
This is usually done at six to eight weeks of pregnancy mainly for those who have had assisted conception or high risk pregnancy. This confirms that pregnancy is in the uterus and excludes ectopic pregnancy, and determines chorionicity (identicalness) of twins. It also establishes the expected date of delivery.
Nuchal Thickness Screening
This occurs between the 11th and 13th week of pregnancy. It determines the risk of Downs Syndrome based on maternal age and appearance of nuchal thickness.
Detailed Anomaly Scan
This occurs between the 22nd and 24th weeks of pregnancy. It is a structured examination of all the major foetal structures and organs including brain, spine, heart, kidneys, bones and umbilical cord. It also includes measurements of head, abdomen and thighs, and can tell you the gender of baby if desired.
Foetal Well-being Scan
If your pregnancy is considered high risk, this scan will be offered between the 32nd and 34th weeks of pregnancy. It measures the foetal head, abdomen and thigh, amniotic fluid volume and cord blood flow.
Diagnosis
Amniocentesis and Chorionic Villus Sampling (CVS) are the main diagnostic procedures for Down’s Syndrome, Edwards’ Syndrome and Cystic Fibrosis. Foetal cells are obtained and analysed for chromosome number and CFTR mutations. Amniocentesis involves inserting a fine needle through the woman’s abdomen into the womb.
A sample of the amniotic fluid surrounding the baby is taken and from this foetal cells are extracted. CVS can be done either by the insertion of a fine needle through the abdomen or through the vagina. A sample is taken of the placenta which comprises foetal cells only.
Both procedures take about ten minutes and are performed on an outpatient basis. Some women may experience slight discomfort. The advantage of CVS is that it can be done earlier in the pregnancy, from about ten weeks. Amniocentesis is usually performed around 16 weeks, although practice varies. Both carry an element of risk and about one in 100 – 200 may miscarry.














